Home → ERCP
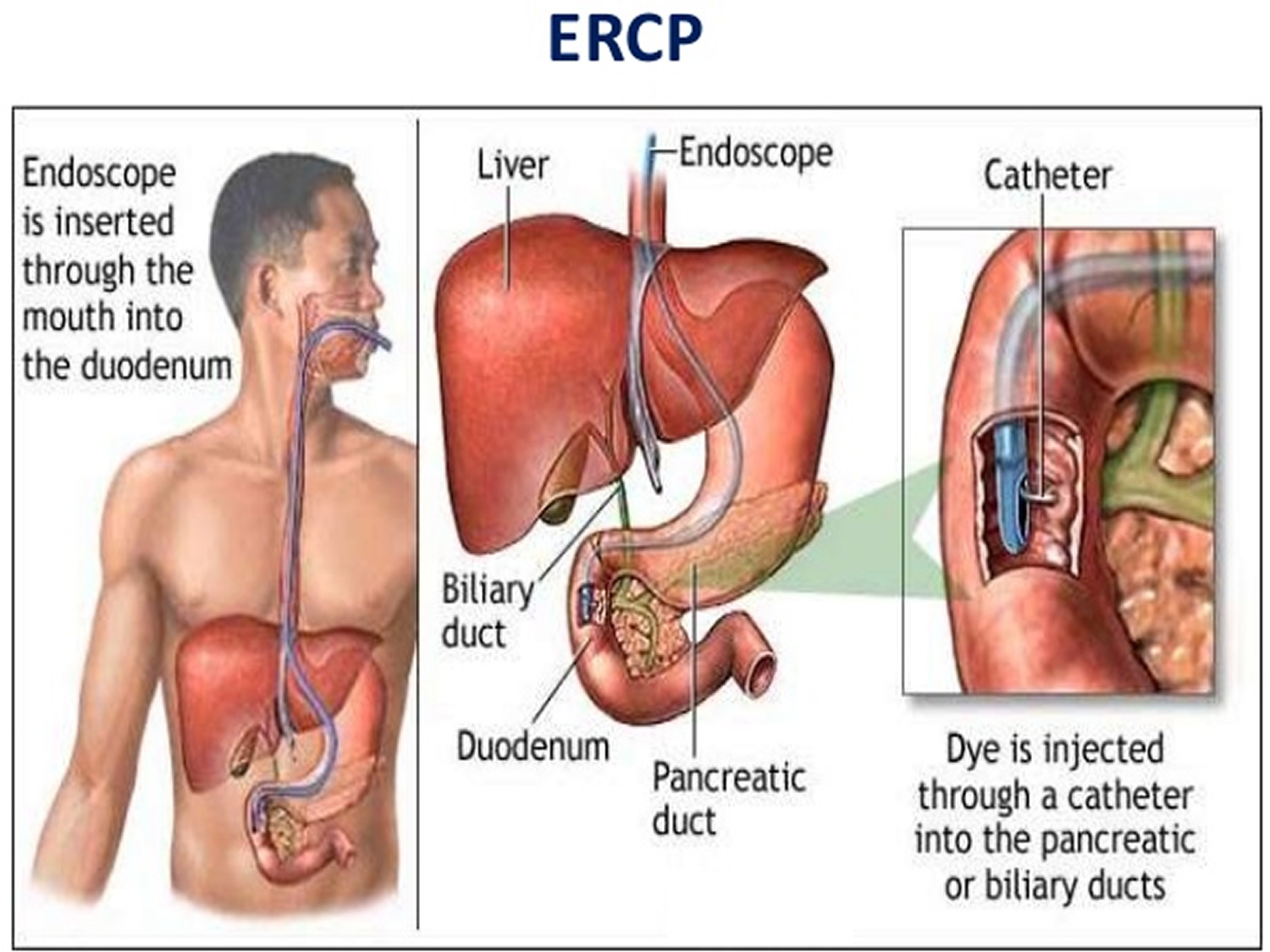
Endoscopic retrograde cholangiopancreatography (ERCP) is a procedure that combines upper gastrointestinal (GI) endoscopy and x-rays to treat problems of the bile and pancreatic ducts.
Your bile ducts are tubes that carry bile from your liver to your gallbladder and duodenum. Your pancreatic ducts are tubes that carry pancreatic juice from your pancreas to your duodenum. Small pancreatic ducts empty into the main pancreatic duct. Your common bile duct and main pancreatic duct join before emptying into your duodenum.
Doctors use ERCP to treat problems of the bile and pancreatic ducts. Doctors also use ERCP to diagnose problems of the bile and pancreatic ducts if they expect to treat problems during the procedure. For diagnosis alone, doctors may use noninvasive tests—tests that do not physically enter the body—instead of ERCP. Noninvasive tests such as magnetic resonance cholangiopancreatography (MRCP)—a type of magnetic resonance imaging (MRI) —are safer and can also diagnose many problems of the bile and pancreatic ducts.
Doctors perform ERCP when your bile or pancreatic ducts have become narrowed or blocked because of
To prepare for ERCP, talk with your doctor, arrange for a ride home, and follow your doctor’s instructions.
Talk with your doctor
You should talk with your doctor about any allergies and medical conditions you have and all prescribed and over-the-counter medicines, vitamins, and supplements you take, including
Your doctor may ask you to temporarily stop taking medicines that affect blood clotting or interact with sedatives. You typically receive sedatives during ERCP to help you relax and stay comfortable.
Tell your doctor if you are, or may be, pregnant. If you are pregnant and need ERCP to treat a problem, the doctor performing the procedure may make changes to protect the fetus from x-rays. Research has found that ERCP is generally safe during pregnancy.1
For safety reasons, you can’t drive for 24 hours after ERCP, as the sedatives or anesthesia used during the procedure needs time to wear off. You will need to make plans for getting a ride home after ERCP.
To see your upper GI tract clearly, you doctor will most likely ask you not to eat, drink, smoke, or chew gum during the 8 hours before ERCP.
Doctors who have specialized training in ERCP perform this procedure at a hospital or an outpatient center. An intravenous (IV) needle will be placed in your arm to provide a sedative. Sedatives help you stay relaxed and comfortable during the procedure. A health care professional will give you a liquid anesthetic to gargle or will spray anesthetic on the back of your throat. The anesthetic numbs your throat and helps prevent gagging during the procedure. The health care staff will monitor your vital signs and keep you as comfortable as possible. In some cases, you may receive general anesthesia.
You’ll be asked to lie on an examination table. The doctor will carefully feed the endoscope down your esophagus, through your stomach, and into your duodenum. A small camera mounted on the endoscope will send a video image to a monitor. The endoscope pumps air into your stomach and duodenum, making them easier to see.
During ERCP, the doctor
After ERCP, you can expect the following:
Following the procedure, you—or a friend or family member who is with you if you’re still groggy—will receive instructions on how to care for yourself after the procedure. You should follow all instructions.
Some results from ERCP are available right away after the procedure. After the sedative has worn off, the doctor will share results with you or, if you choose, with your friend or family member.
If the doctor performed a biopsy, a pathologist will examine the biopsy tissue. Biopsy results take a few days or longer to come back.
The risks of ERCP include complications such as the following: