Home → Infected sebaceous cyst excision
Epidermoid cysts are asymptomatic, dome-shaped lesions that often arise from a ruptured pilosebaceous follicle. The minimal excision technique for epidermoid cyst removal is less invasive than complete surgical excision and does not require suture closure. The procedure is easy to learn, and most physicians experienced in skin surgery can perform the procedure after three to five precepted sessions. It involves making a 2- to 3-mm incision, expressing the cyst contents through compression and extracting the cyst wall through the incision. Gauze or a splatter shield should be used to protect the physician from spraying of cyst contents. The rarity of associated cancer makes histologic evaluation necessary only if unusual findings or clinical suspicion of cancer is present. Inflamed cysts are difficult to e excise, and it is often preferable to postpone excision until inflammation has subsided.
Epidermoid cysts are asymptomatic, slowly enlarging, firm-to-fluctuant, dome-shaped lesions that frequently appear on the trunk, neck, face, scrotum or behind the ears. Occasionally, a dark keratin plug (a comedo) can be seen overlying the cyst cavity. These epithelial, walled cysts vary from a few millimeters to 5 cm in diameter. The cysts are mobile unless fibrosis is present.
The term “sebaceous cyst” has fallen into disuse; current terms include epidermal cyst, keratin cyst, epithelial cyst, and epidermoid cyst. Other types of cysts are included in Table 1. Epidermoid cysts often arise from a ruptured pilosebaceous follicle associated with acne. Duct obstruction of a sebaceous gland in the hair follicle can result in a long, narrow channel opening in the surface comedo. Other causes include a developmental defect of the sebaceous duct or traumatic implantation of surface epithelium beneath the skin.
The cysts contain keratin and lipid, and the rancid odor often associated with these cysts relates to the relative fat content, bacterial infection, or decomposition. Spontaneous rupture discharges the soft, yellow keratin material into the dermis. A tremendous inflammatory response (foreign-body reaction) ensues, often producing a purulent material. Scarring makes removal more difficult.
Most cysts are simple lesions, but a few special situations should be considered. Multiple epidermoid cysts (associated with lipomas or fibromas of the skin) and osteomas should be considered as part of Gardner's syndrome, with associated premalignant colonic polyps. Dermoid cysts of the head often can be confused with epidermoid cysts, and attempted removal of a dermoid cyst can create a wound with Excision and closure of epidermoid cysts can be difficult if inflammation is present; it may be preferable to postpone excision until the inflammation has subsided. intracranial communication. Some cysts can be associated with basal cell and squamous cell carcinoma, and some authors advocate histologic evaluation of the wall of all removed cysts. The rarity of associated cancer makes routine histologic evaluation necessary only when solid tumors or unusual findings are present.
Cyst infection can develop spontaneously or following rupture. It is often unclear whether an inflamed cyst is infected, and many physicians prefer to treat these lesions with antibiotics, incision, and drainage. Excision and closure can be very difficult with inflamed cysts, and it may be preferable to postpone the surgical procedure until the inflammation has subsided (typically one week).
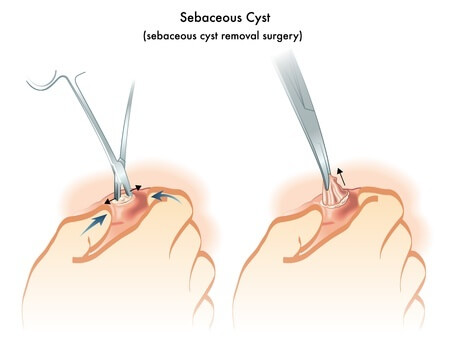
There are many surgical approaches to epidermoid cysts. While complete surgical excision can ensure removal of the sac and prevent recurrence, this technique is time-consuming and requires suture closure. The minimal excision technique has been proposed as a less invasive and successful intervention. The minimal excision technique involves a 2- to 3-mm incision, expression of the cyst contents, and extraction of the cyst wall through the incision. Vigorous finger compression is used to express the cyst contents and loosen the cyst wall from the surrounding tissues to facilitate removal of the sac. The tiny wound can be closed with a single suture, although most physicians do not close this opening. A variation of this technique uses a punch biopsy instrument to create the opening into the cyst.
Expression of the cyst contents through the small opening can cause the sebaceous material to spray across the surgery room. Gauze can be used to cover the area as compression is applied, or a clear adhesive splatter-control shield can be used to cover the site. Some practices require the use of protective eye wear for the procedure.
Simple incision and drainage of cysts frequently results in recurrence. Two iodine crystals can be placed in the center of the cyst and, during the next few weeks, the cyst will become dark brown and hard. This hard nodule can then be expressed from the skin. This simple technique is inexpensive, but the need for a follow-up visit and the length of time for lesion removal may make this technique less desirable to many patients.